What is ALS
For year 2014, social media was awash with people getting a ice bucket water dumped over them while they nominated other to do likewise, all to raise money and awareness for Amyotrophic Lateral Sclerosis (ALS). Also known as Lou Gehrig’s Disease in America (after its most famous sufferer, baseball star Lou Gehrig), this neurodegenerative disease is an insidious killer, where sufferer have a typical life-expectancy of three years from the date of contracting the illness. Even more chilling, there is no cure for als disease, although some symptoms of als may be controlled.
Discovered by French neurologist
Jean-Martin Charcot in 1869, the most common form of ALS is sporadic, meaning
it strikes randomly. The other type of ALS, “familial”, is hereditary, whereby
there is a 50% chance that children of those affected by ALS will have the gene
mutation, and thus, develop the als disease.
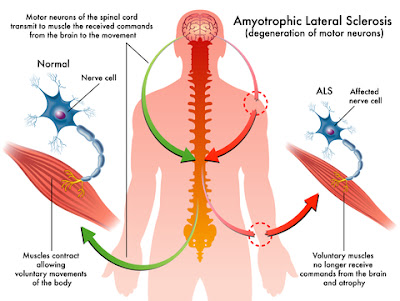
The inescapable feature seen in ailing
victims is the progressive decline of muscle control, and thereby, voluntary
movement. This occurs because nerve cells responsible for person’s motor
capacity are malfunctioning.
When upper motor neuron (found in the
brain) die, they stop signaling the spinal cord to initiate and control muscle
movement. Meanwhile, impaired lower motor neuron (found in the lateral regions
of the spinal cord) causing scarring or hardening (sclerosis) of the spinal
cord, which also disrupt signaling to muscles. Owing to the continuous degeneration
of both motor neurons, muscles atrophy, and the victim deteriorates physically,
gradually losing abilities like moving, eating, speaking and eventually,
breathing.
The general age bracket for susceptibility
is between 40 and 70 years old. Interestingly, a study by US Department of
Veteran Affairs showed that those deployed during the 1991 Gulf War are twice as
vulnerable to the disorder compared to the general public.
ALS Diagnosis
In the early stage of ALS, symptoms of ALS
can be easily confused with those of other diseases and disorders such as human
immunodeficiency virus (HIV), human T-cell leukemia virus (HTLV), polio, West
Nile virus and Lyme disease. Physicians also consider the possibility of neurological
disorders such as multiple sclerosis, post-polio syndrome, multifocal motor
neuropathy and spinal muscular atrophy; all of which can mimic characteristics
of the disease.
Hence, appropriate assessments are carried
out to eliminate these possible conditions before drawing ALS as conclusion.
Such test include an electromyography (EMG) to detect electrical activity in
muscles, a nerve conduction study (NCS) to assess nerve signals, and a magnetic
resonance imaging (MRI) scan which may substantiate the presence of other
problems. Based on the findings, blood and urine samples are analyzed alongside
other routine laboratory testing.
ALS begins very subtly and symptoms of ALS
are difficult to perceive. General cramps, stiffness, muscle weakness in either
arms or legs, slurred speech or difficulty in chewing or swallowing are among
initial onset signs, but are easily interpreted as non-related.
When muscles in limb are affected, victims
suddenly find themselves losing manual dexterity. Simple task like turning a
key, buttoning a shirt and writing, for example, become difficult and walking
or running feels awkward as they trip and stumble often. Then there are those
who initially experience speech problem.
As the ALS disease advances, muscle atrophy
spreads to other parts of body, and becomes more defined. Spasticity (unusual
muscle tightness) and exaggerated reflexes indicate upper motor neuron damage,
while lower motor neuron degeneration includes severe muscle weakness, cramps
and fasciculation (flickering movements under the skin).
The rate of ALS disease progresses varies
between individuals. But they all reach the unfortunate point of being in a
vegetative state when limbs cease to function, and they are unable to eat
without choking. Still cognitive and lucid, they behold their own steady
destruction helplessly. In the last stages, the ability to breath diminishes as
the muscles of the respiratory system weaken, thus they require a ventilator to
breath.
ALS treatment
There is no cure for ALS, only the use of
certain drugs to control symptoms of als. Riluzole provides modest benefits sufferers
by delaying the onset of ventilator-dependence, and prolonging the survival of
those with difficulty in swallowing, by several months. However, throwbacks
include increased risk of liver damage and side effects, among which are allergic
reactions (skin problems, chest tightness, swelling of lips, tongue and throat,
fever, irregular heartbeat, jaundice, nausea, stomach problems and flu-like
symptoms.
Physicians can also prescribe medication to
help alleviate fatigue, muscle cramps, spasticity, and to lessen the excess
saliva and phlegm produced. Drugs to relieve pain, depression, sleep
disturbances and constipation may also be given but care is taken to prevent
risky interactions.
Physical therapy is another ALS treatment
aspect. Unaffected muscles are strengthened with low-impact aerobic exercises
like walking, swimming and stationary bicycling, which also improve
cardiovascular health and mood. On the social side of things, speech therapists
provide adaptive strategies to speak louder and clearer, as well as techniques
to respond non-verbally. Speech synthesizers and computer-based communication
systems can be vital devices for those who have shutdown vocally.